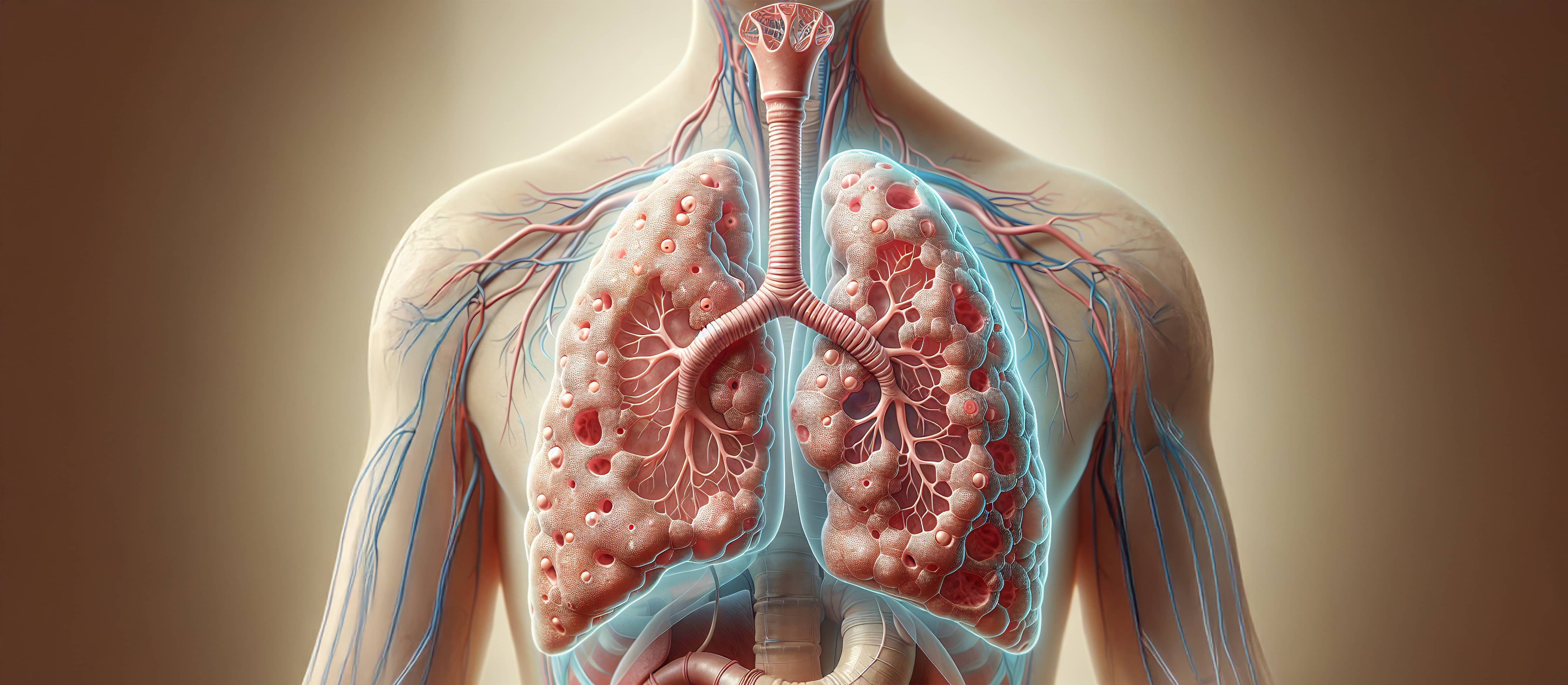
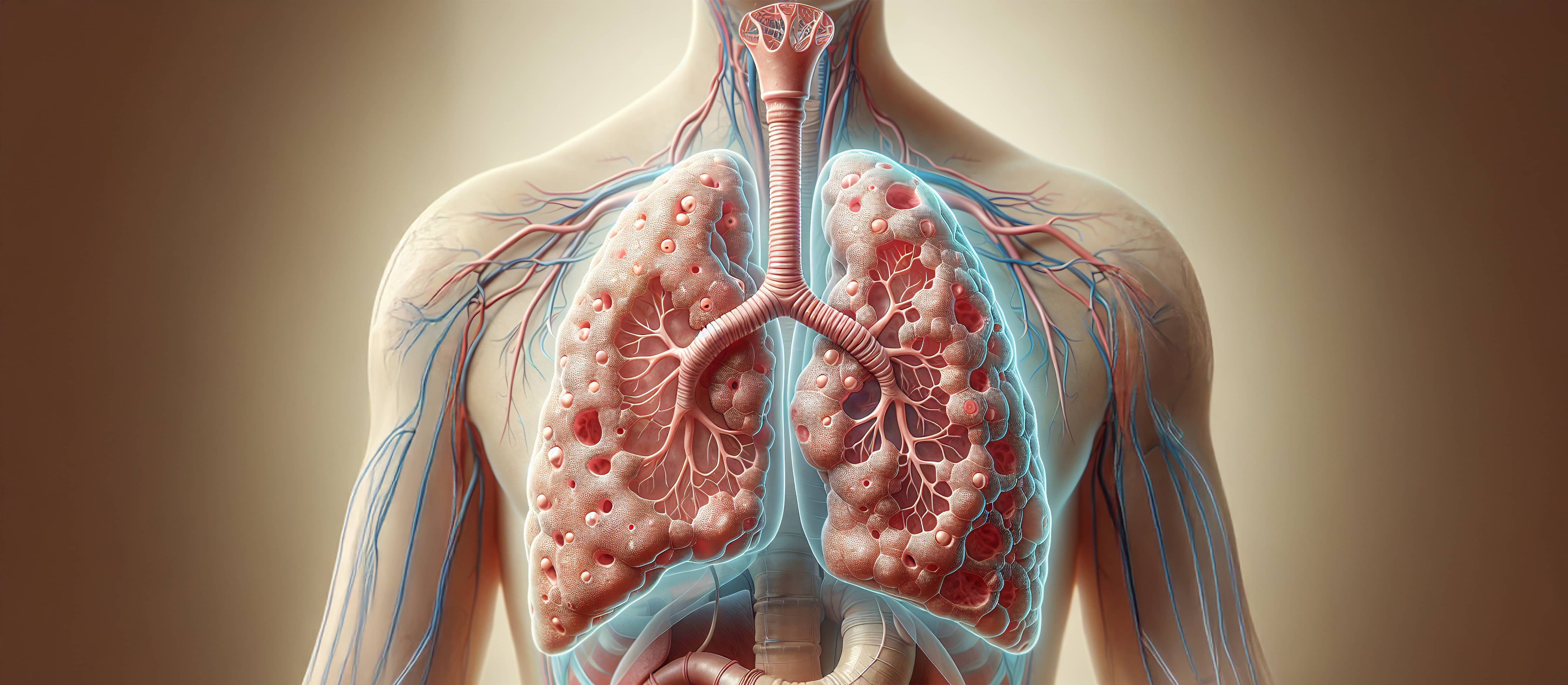
Idiopathic Pulmonary Fibrosis (IPF) remains a significant clinical challenge—marked by progressive scarring, limited treatment options, and a lack of reliable biomarkers. These hurdles slow drug development and increase the risk of late-stage failure. What’s needed is an integrated framework—one that connects preclinical modeling with molecular and morphological data to enable smarter, faster, and more predictive drug development.
At Aragen, we provide an integrated, translational framework that bridges robust preclinical modeling with molecular and histological insights, enabling early biomarker discovery, targeted therapeutic evaluation, and confident, data-driven decision-making.
The development of impactful therapeutics relies on disease models that accurately replicate human pathophysiology. Robust preclinical data lay the groundwork for successful clinical translation.
Aragen offers optimized, reproducible bleomycin-induced pulmonary fibrosis models with both acute and chronic models well established. These models capture hallmark features of IPF—such as alveolar damage, inflammatory infiltration, and collagen deposition—and deliver consistent outputs including lung weight increases, bronchoalveolar lavage (BAL) cell influx, and elevated levels of chemokines such as MCP-1 and IP-10—features often correlated with human fibrotic pathology. The chronic model is increasingly becoming relevant because of the presence of persistent fibrosis in the lungs, along with gradual resolution of inflammation, as determined by histological and transcriptomic analyses across both acute and chronic models. Notably, FDA-approved drugs for IPF—Pirfenidone and Nintedanib have been evaluated in both acute and chronic models, showing improvement in both in-life as well as ex vivo parameters.
These translationally relevant models have supported efficacy studies and IND filings across small molecules, biologics, and RNA therapeutics. Aragen’s fibrosis research capabilities extend beyond lung fibrosis to other fibrotic diseases, including liver, kidney, skin, scleroderma, and metabolic dysfunction-associated steatohepatitis (MASH), expanding the scope of research by enabling cross-organ comparisons. This integrated, system-wide perspective helps uncover shared mechanisms of fibrosis and guides biomarker discovery with stronger translational potential.
Understanding the molecular mechanisms underpinning fibrosis is critical to identifying candidate biomarkers and therapeutic targets. Aragen applies a curated panel of fibrosis-related genes focused on key fibrogenic pathways such as:
These expression profiles allow for sensitive detection of molecular changes across preclinical models. By applying this panel across lung, liver, kidney, and skin fibrosis models, Aragen has helped delineate both conserved and tissue-specific gene signatures, providing insight into shared disease mechanisms and informing cross-organ biomarker development.
For example, gene expression profiling has revealed parallels in TGF-β activation and collagen gene upregulation in both lung and liver models, contributing to a more unified understanding of systemic fibrotic processes.
Traditional histological scoring is often limited by subjectivity and low reproducibility. Aragen addresses this by applying AI-driven digital pathology platform (Visiopharm) to lung tissue sections. This system enables high-resolution, algorithm-based quantification of:
In fibrosis models, this quantitative spatial analysis complements molecular readouts and enhances detection of treatment-related changes. For instance, AI pathology can detect subtle improvements in fibrotic burden that may precede changes in lung function—offering an earlier and more sensitive endpoint for efficacy assessment.
Successful translation from bench to bedside hinges on integrating multiple efficacy endpoints. Aragen incorporates multiple readouts to evaluate therapeutic impact, including:
This integrated approach enables assessment at molecular, functional, and structural levels. A recent example includes studies evaluating ALK5 (TGF-β receptor) inhibitors, where gene suppression, reduced collagen deposition, and improved lung mechanics were all observed—illustrating the translational value of combining orthogonal readouts.
To complement in vivo modeling, Aragen provides supporting in vitro and ex vivo systems to elucidate specific cellular and molecular mechanisms. These include:
These platforms enable high-throughput screening, mechanistic interrogation, and validation of fibrosis-related targets in a controlled environment—supporting more informed progression to in vivo studies.
The path from preclinical discovery to clinical translation in IPF is not linear—it relies on a continuous feedback loop between models, markers, and measurement tools. This nexus, built on validated fibrosis models, targeted molecular profiling, spatial tissue analysis, and diverse efficacy endpoints, provides an integrated framework for identifying meaningful biomarkers and understanding therapeutic mechanisms in context. This holistic approach supports:
By linking disease models to measurable markers, researchers gain the ability to detect subtle biological changes, refine therapeutic hypotheses, and improve confidence in translational relevance.
Whether you are exploring early-stage targets or advancing toward IND, Aragen enables translate data into decisions—moving therapies from the lab toward the clinic with confidence. Our end-to-end platform combines scientific depth with operational agility—offering:
Discover more about Aragen’s fibrosis capabilities and collaborate now to advance your fibrosis research.
